UMC Utrecht develops 3D-printed mold for better treatment of nasal cancer
Researchers at UMC Utrecht have developed an innovative 3D printed mold that makes nasal cancer treatment more accurate and patient-friendly. Thanks to the customized mold, tumors can be irradiated more precisely. This results in less damage to surrounding tissue and faster recovery.
Radiation is an effective cancer treatment, but the radiation often causes side effects as it passes through the body. Surrounding, healthy tissue therefore suffers unwanted radiation effects. Especially with cancer in the head and neck area, where practitioners have to deal with a lot of sensitive tissue near the tumor, this often causes side effects. Every year, 50 to 60 people are diagnosed with nasal cancer.
Treatment for nasal cancer
This radiation damage can be reduced by using internal radiation therapy. In this so-called brachytherapy, practitioners place the radioactive source inside or as close to the tumor as possible through tubes. The technique causes less damage to the surrounding tissue, and is therefore used for tumors in the head and neck area whenever possible.
The technique works as follows: healthcare workers puncture holes in the nose up to close to the tumor, into which small tubes or tubing fit. These accommodate a cable with a radioactive source attached. A computer program determines which tube the cable runs through and how long the radioactive source remains in place. The treatment is finished when the desired amount of radiation is reached, usually after about five minutes. This is repeated once or twice a day for up to a week and a half.
Improving therapy
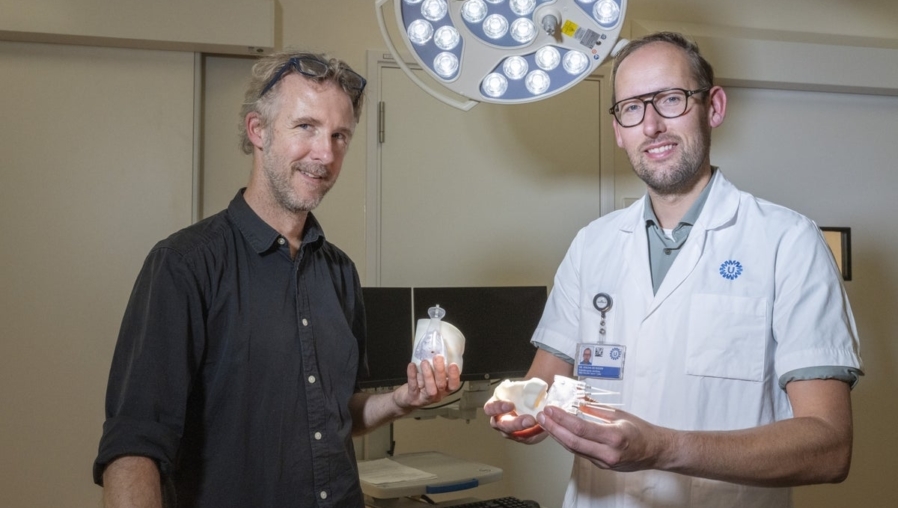
The technique works well, but is often uncomfortable for the patient, says Mischa de Ridder, radiotherapist-oncologist at UMC Utrecht. “We always try to irradiate the tumor as well as possible with as little tissue damage as possible by puncturing the holes. Still, in addition to radiation damage, puncturing the holes can also cause damage to the nose.” Together with his colleagues, he therefore improved the therapy. They designed a nasal mold, which they 3D printed to size for each patient. This allows practitioners to place the tubes as precisely as possible, and it is possible to achieve the same goal with fewer tubes.
Research by De Ridder and his colleagues shows that the mold offers a better and more effective way to treat people with nasal cancer. “In almost everyone who underwent the treatment, the radiation reached the tumor very accurately, after which the tumor disappeared and the nose could be preserved.” In the process, patients experienced fewer side effects, as the radiation did not target surrounding tissues and practitioners needed to puncture fewer holes in the nose.
3D printed mold
Designing the mold is the job of Maarten Kastelijns, a radiotherapy lab technician at UMC Utrecht. He specializes in designing the 3D prints for brachytherapy. “Based on medical imaging, together we make a plan to place the tubes as close to the tumor as possible. The lab technicians design a mold around that from a type of plastic.” That mold consists of a base part that fits as closely as possible around the patient’s nose, and has several components. “It has adhesive holes to attach the mold to the nose, and a mechanism that allows us to attach the tubes to the mold.”
The mold stays in place during treatment, allowing practitioners to administer an optimal amount of radiation. This can be uncomfortable for the patient, though. “Thanks to the mold, the treatment plan remains guaranteed,” Kastelijns says. “Puncturing the holes and attaching the mold can be painful. That’s why we do it under anesthesia. Once the patient is awake, the pain is usually not too bad. Paracetamol is often enough to accomplish the treatment.”
Fast recovery process
Because the mold stays in place, many patients experience nasal congestion symptoms, De Ridder says. “They feel like they have a cold for a week. With the mold you can’t blow your nose, so we printed holes in it to administer nasal spray. They can still pick their nose then.” When the mold goes off the nose after treatment, it often feels like a relief. “The snot and mucus finds a way out when suddenly they can breathe through their nose again,” he says.
After that, the recovery process can begin. “Releasing the sutures is quick and easy and similar to removing an IV. We just do that in the treatment room, without anesthesia,” says De Ridder. During the period afterward, the nose reacts to the radiation treatment. “That’s often an unpleasant period, because people get scabs in the nose that quickly start to bleed. But after about six weeks, the tumor is gone and the inside of the nose has already healed.”
Welcome addition
Thanks to the positive results, the researchers see potential to use molds for other tumors not currently treated with brachytherapy, for example nasopharyngeal cancer. “For that type of treatment, we never had suitable molds,” says Kastelijns. “That is possibly going to change now that we are able to make them ourselves. Depending on the mold and application, we can even vary the material to be printed. We don’t yet know what is the best method per indication, but we see many applications in the future, especially in the head and neck area.”
“Brachytherapy provides a much nicer dose distribution, where you save so much more tissue than with other techniques,” says De Ridder. “We’ve treated about 10 patients for years, but with the addition of the molds and their results, we’re seeing that number increase. If we can perfect this technique even further, that would be a welcome addition for patients.”